Diagnostic Ambiguity and Mismedicine in Generalized Anxiety Disorder
Introduction:
Generalized anxiety disorder (GAD) is a mental health condition characterized by excessive and persistent worry that interferes with everyday life and is experienced by patients as difficult to control (Kong & Zhang, 2025). This pattern of anxiety is typically sustained for six months or longer. It is accompanied by a range of physical, cognitive, and emotional symptoms, including muscle tension, difficulty concentrating, and sleep disturbances (Matsuyama et al., 2024).
Prevalence:
According to the DSM-5, GAD demonstrates notable global disparities in prevalence, with higher rates observed in high-income countries (approximately 5%) compared with low-income countries (1.6%), and an overall lifetime prevalence of 3.7% (Hurtado et al., 2020). Thereby, it highlights global disparity in the recognition, diagnosis, and reporting of anxiety disorders.
Neurobiological Correlates of Anxiety Dysregulation:
Neuroimaging studies further suggest that GAD is associated with altered brain activity and functional connectivity, including reduced resting-state connectivity between the amygdala and prefrontal cortex, as well as abnormal connectivity involving the anterior cingulate cortex; neural patterns implicated in threat processing and emotion regulation (Patriquin & Mathew, 2017). Therefore, this reduction in connectivity may lead individuals to exhibit variability in how they perceive threats and; in their ability, to select appropriate physiological, emotional, and cognitive responses that match the contextual demands of a situation.
Mismedicine; Diagnostic Ambiguity and the “Wastebasket” Diagnosis:
In the context of generalized anxiety disorder, diagnostic ambiguity and treatment misalignment may be understood through the lens of Mismedicine, a term coined by Dr. Pooya Beigi which describes medical actions that result in inefficiency or a failure to meet the standard of care; misdiagnosis represents one manifestation of this phenomenon (MARI, 2022). In addition, GAD may function as a “wastebasket” diagnosis when clinical presentations are nonspecific or do not clearly meet criteria for other psychiatric disorders, increasing the risk of overdiagnosis (Matsuyama et al., 2024). Such diagnostic imprecision may contribute to treatment of mismatch, reduced patient satisfaction, and diminished confidence in recovery, while also complicating the interpretation of prevalence estimates and treatment outcomes. From a systems perspective, these challenges may further contribute to inefficient resource allocation and prolonged treatment pathways within healthcare settings (Hurtado et al., 2020). Hurtado et al. (2020) additionally report limited patient involvement in treatment decision-making, with pharmacological interventions prioritized despite the multifaceted nature of anxiety disorders. Although medication may reduce symptom severity, anxiety disorders reflect an interaction between physiological dysregulation and maladaptive coping mechanisms, suggesting that integrated, patient-centred treatment approaches may be more holistic.
Methodological Implications of Diagnostic Misclassification:
Due to diagnostic ambiguity and potential misclassification, reported prevalence rates and treatment outcomes may not accurately reflect the true burden or clinical course of GAD. Conceptually, diagnostic ambiguity in GAD may initiate a cascade in which symptom overlap leads to misclassification, misclassification contributes to treatment mismatch, and treatment mismatch reinforces persistent impairment and reduced patient engagement.
Inter-Individual Variability and Sociocultural Influences on Symptom Expression:
Research (Kong & Zhang, 2025) has demonstrated inter-individual variability in anxiety-related responses. Inter-individual variability refers to systematic differences across individuals in the experience and expression of anxiety symptoms, shaped by psychological, biological, and sociocultural factors. For example, gender differences have been documented in both self-reported anxiety symptoms and stress vulnerability, with females consistently reporting higher levels of anxiety and demonstrating heightened sensitivity to stress relative to males (Kong & Zhang, 2025). Cultural differences in anxiety symptom reporting have also been identified, whereby Black/African American participants report lower levels of generalized anxiety on the GAD-7 than White/Caucasian and Hispanic participants, despite experiencing comparable levels of anxiety symptoms (Kong & Zhang, 2025). These differences suggest that standardized self-report measures may inadequately capture anxiety experiences across diverse populations, thereby introducing systematic bias into clinical assessment. Such inter-individual and sociocultural variability may further complicate symptom-based diagnostic assessment and contribute to diagnostic misclassification.
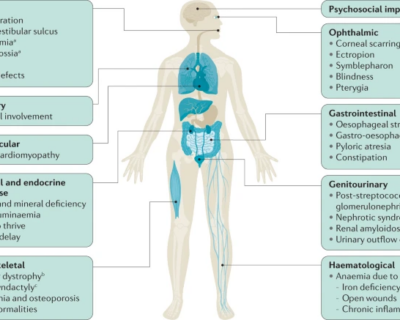
Comorbidity, Somatic Manifestations, and Medical Mimics:
The high comorbidity between generalized anxiety disorder (GAD) and panic disorder (PD) may be partly explained by shared dysfunction in limbic–prefrontal circuitry, including the amygdala, which underlies heightened threat sensitivity and somatic manifestations of anxiety (Caldiroli et al., 2023). These shared somatic features, such as palpitations, muscle tension, and autonomic arousal, can blur diagnostic boundaries between anxiety disorders (Caldiroli et al., 2023). More broadly, the existence of multiple anxiety disorder subtypes with overlapping symptom profiles shows how common physiological pathways can produce similar clinical presentations across diagnostic categories. Importantly, anxiety-like somatic symptoms may also arise from certain medical conditions, such as thyroid dysfunction, which can mimic psychiatric anxiety presentations and further increase the risk of diagnostic confusion within symptom-based diagnostic frameworks (Caldiroli et al., 2023).
Conclusion:
In conclusion, Generalized Anxiety Disorder is a prevalent yet diagnostically complex condition, characterized by symptom overlap with other anxiety subtypes, inter-individual variability shaped by cultural and gender differences, and frequent comorbidity with other psychiatric and medical conditions. If healthcare systems rely heavily on symptom-based diagnostic frameworks, the risk of misclassification may increase, thereby complicating prevalence estimates and the interpretation of treatment outcomes. These challenges underscore the need for greater diagnostic precision and integrative, patient-centred approaches that account for neurobiological mechanisms, individual symptom profiles, and sociocultural influences. Therefore, improving methodological rigor and diagnostic clarity is essential for advancing both research and clinical care in GAD.
References
Caldiroli, A., Colzani, L., Capuzzi, E., Quitadamo, C., La Tegola, D., Surace, T., Russo, S., Capetti, M., Leo, S., Tringali, A., Marcatili, M., Zanelli Quarantini, F., Colmegna, F., Dakanalis, A., Buoli, M., & Clerici, M. (2023). Clinical Markers of Panic and Generalized Anxiety Disorder: Overlapping Symptoms, Different Course and Outcome. Journal of Personalized Medicine, 13(3), 491. https://doi.org/10.3390/jpm13030491
Hurtado, M. M., Villena, A., Vega, A., Amor, G., Gómez, C., & Morales‐Asencio, J. M. (2020). “I have anxiety, but I have values and preferences” Experiences of users with generalized anxiety disorder: A qualitative study. International Journal of Mental Health Nursing, 29(3). https://doi.org/10.1111/inm.12690
Kong, L., & Zhang, L. (2025). An Alternative Approach to Future Diagnosis: Can Generalized Anxiety Disorder Be Distinguished From Major Depressive Disorder, Healthy People by Differentially Expressed lncRNAs in Peripheral Blood. Neuropsychiatric Disease and Treatment, Volume 21, 729–739. https://doi.org/10.2147/ndt.s511375
MARI. (2022, February 17). Our Organization | Misdiagnosis Association and Research Institution. MARI | Misdiagnosis Association and Research Institution. https://mariresearch.com/our-organization/
Matsuyama, S., Otsubo, T., Nomoto, K., Higa, S., & Takashio, O. (2024). Prevalence of Generalized Anxiety Disorder in Japan: A General Population Survey. Neuropsychiatric Disease and Treatment, Volume 20, 1355–1366. https://doi.org/10.2147/ndt.s456272
Patriquin, M. A., & Mathew, S. J. (2017). The Neurobiological Mechanisms of Generalized Anxiety Disorder and Chronic Stress. Chronic Stress, 1(1), 247054701770399. https://doi.org/10.1177/2470547017703993
Provided and edited by the members of MARI Research, Error in Medicine Foundation and MISMEDICINE Research Institute, including Emilia Jianing, Charmi Patel, and Dr. Pooya Beigi MD. MSc.