SSRIs and Major Depression Disorder: Effectiveness, Harms, and Practical Steps to Avoid Mismedicine
Selective serotonin reuptake inhibitors (SSRIs) are among the most commonly prescribed pharmacological treatments for major depressive disorder (MDD) and remain a first-line option in many guidelines (Gabriel et al., 2020; Jakobsen et al., 2017). However, increasing scrutiny of antidepressant outcomes has raised important questions about the magnitude of SSRI benefits and adverse effects, and whether current prescribing practices optimally balance benefit and harm (Jakobsen et al., 2017). This issue is particularly significant given the progressively increasing worldwide impact of depression (Moreno-Agostino et al., 2021).
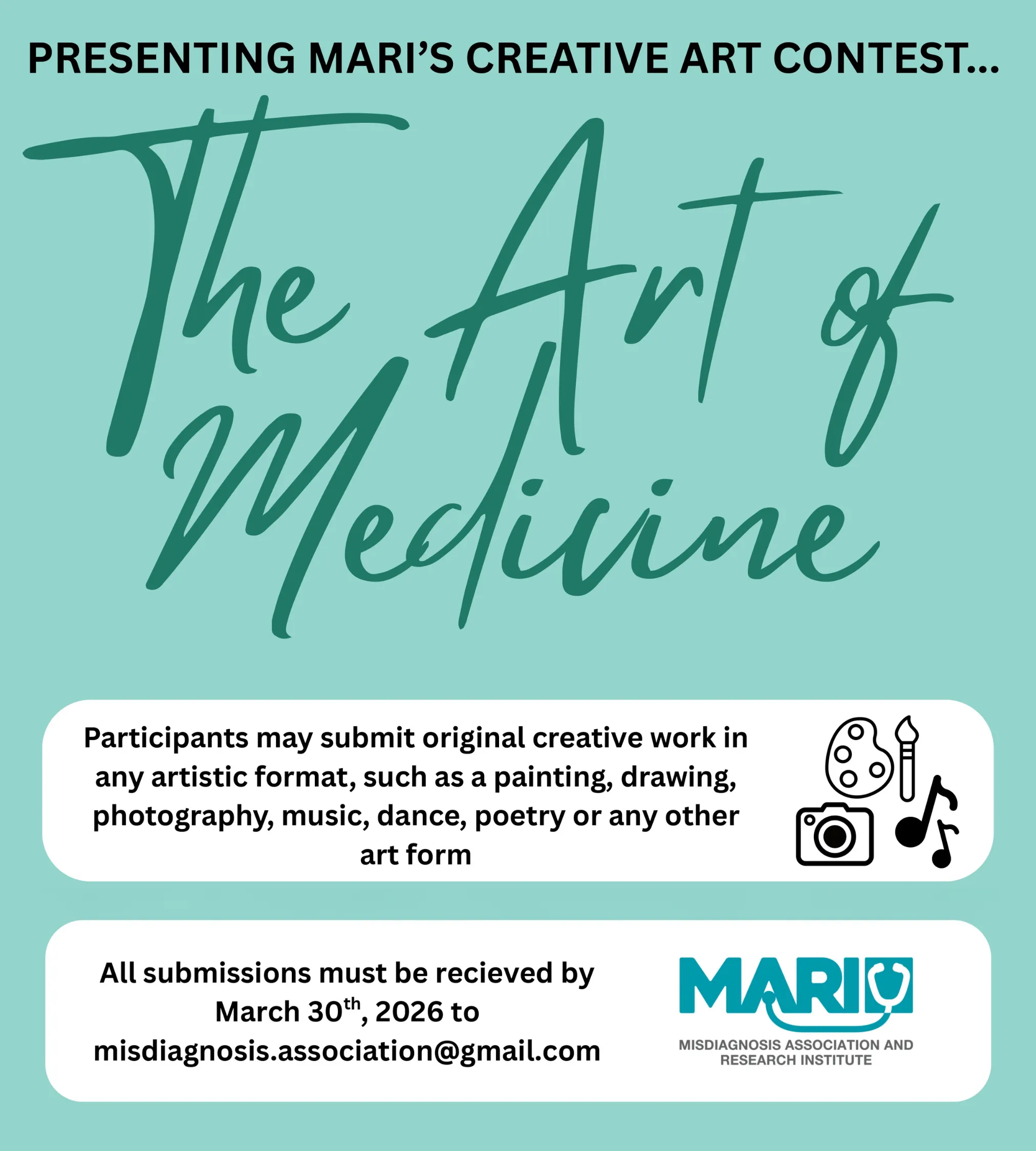
As prevalence grows and SSRIs continue to be regularly recommended, safe and evidence-based SSRI prescribing is therefore essential to maximize benefit and minimize harm (Gabriel et al., 2020; Jakobsen et al., 2017; Moreno-Agostino et al., 2021). This review critically examines the overall benefits and risks of SSRIs in the treatment of major depressive disorder and explores how current evidence can inform practical suggestions that support safer prescribing, reducing potential “mismedicine.” Dr. Pooya Beigi, founder of the Misdiagnosis Association and Research Institute (MARI), has coined this term to broadly and comprehensively explain medical acts that produce harm, inefficiency, or failure to meet the standard of care, such as diagnostic, therapeutic, communicative, or system errors (Beigi, 2019).
What are SSRIs and How Do They Work?
SSRIs are a class of antidepressants that include specific medications like fluoxetine, sertraline, citalopram/escitalopram, paroxetine, and fluvoxamine (Edinoff et al., 2021). They work by blocking the brain’s process of reabsorbing serotonin, a neurotransmitter involved in mood regulation, increasing its availability and allowing for it to remain active for longer (Edinoff et al., 2021; Ferguson, 2001). SSRIs can be used across the acute phase (treating the current depressive episode), the continuation phase (continuing the medication after improvement to prevent relapse), and the maintenance phase (prolonged use to reduce future risk) of depression treatment, frequently being coupled with psychotherapy or other pharmacologic agents (Gabriel et al., 2020; Gautam et al., 2017). Although they share a pharmacological family label, particular SSRIs differ in elements like effects, mechanisms, and tolerability (Edinoff et al., 2021). This variability underscores the importance of careful, evidence-informed prescribing practices.
Prevalence and Relevance
As lightly mentioned, MDD represents a significant and growing source of impairment on a global level (Gabriel et al., 2020; Moreno-Agostino et al., 2021). Work by Gabriel et al. (2020) and Moreno-Agostino et al. (2021) suggests that rates of depression have progressively risen, with estimates putting the number of people affected in the hundreds of millions, indicating a broad upward trend in prevalence over recent decades. As the reach of MDD expands, the need for treatments that are not only effective but also appropriately prescribed becomes a notable clinical and public health priority (Moreno-Agostino et al., 2021). In turn, SSRI prescribing has grown, with this antidepressant class being used for a range of psychiatric conditions extending beyond depression (Edinoff et al., 2021; Jakobsen et al., 2017). This means that even modest benefits or relatively uncommon adverse effects can still affect large numbers of people.
Benefits of SSRIs for Depression
Typically, research finds that SSRIs outperform placebos, being more effective in reducing depressive symptoms and increasing remission rates in adults with MDD, likely underpinning their popular recommendation as first-line treatments (Jakobsen et al., 2017). Many studies indicate that SSRIs may be better for atypical depression symptoms than particular types of antidepressants, which might also factor into increased prescribing (Gautam et al., 2017). Collectively, these findings explain why SSRIs remain central to contemporary pharmacological intervention for patients with moderate-to-severe depression. Despite these advantages, there is evidence that questions the balance between their pros and cons.
Limitations and Potential Mismedicine
Jakobsen et al. (2017) examined many randomized trials and found that the average symptom reduction with SSRIs, while statistically significant, is modest and often falls below predefined thresholds for clinical meaningfulness on standard rating scales. Additionally, many trials are affected by methodological limitations, including risk of bias and short follow-up periods, which may overestimate SSRI’s overall benefit (Jakobsen et al., 2017). Importantly, there are reports of higher rates of adverse events among patients treated with SSRIs compared to placebo groups, including both non-serious and serious harms, with common side effects like nausea, sleep difficulties, agitation, and sexual problems (Edinoff et al., 2021; Ferguson, 2001; Jakobsen et al., 2017; Santarsieri & Schwartz, 2015).
Furthermore, there are important safety concerns, such as interactions with other medications, heart issues with some SSRIs, and increased suicidality risk in younger people, further emphasizing the need for clinician vigilance to avoid mismedicine (Edinoff et al., 2021; Gabriel et al., 2020). Although guidelines converge on SSRI use as a front-line option, they vary in recommendations in aspects like treatment augmentation and suicide-risk management, which can leave clinicians uncertain about the best strategy, possibly contributing to inconsistent care and mismedicine (Gabriel et al., 2020).
Taken together, the widespread use of SSRIs, differences between individual drugs, and mixed evidence about their overall benefits suggest the need for a careful, patient-centred approach to prescribing (Edinoff et al., 2021; Gabriel et al., 2020; Jakobsen et al., 2017). This means selecting medications with attention to drug interactions and heart-related risks, combining medication with psychotherapy when appropriate, and setting realistic expectations about symptom improvement (Gabriel et al., 2020). Regular follow-ups and early safety checks may also help to identify side effects or lack of response. Improving prescribing practices in this way can facilitate guideline recommendations that translate into safer and more consistent care for patients.
Conclusion
Selective serotonin reuptake inhibitors occupy a central yet contested position in the treatment of major depressive disorder, reflecting their common use alongside ongoing debate about their true clinical value and safety. Thoughtful prescribing where individual needs are considered and follow-up monitoring are therefore essential and may reduce harm, limiting possible mismedicine.
References
Beigi, P. (2019, February 20). The Misdiagnosis Association and Research Institution (MARI). MARI. https://mariresearch.com/
Edinoff, A. N., Akuly, H. A., Hanna, T. A., Ochoa, C. O., Patti, S. J., Ghaffar, Y. A., Kaye, A. D., Viswanath, O., Urits, I., Boyer, A. G., Cornett, E. M., & Kaye, A. M. (2021). Selective Serotonin Reuptake Inhibitors and Adverse Effects: A Narrative Review. Neurology International, 13(3), 387–401. https://doi.org/10.3390/neurolint13030038
Ferguson, J. M. (2001). SSRI antidepressant medications: Adverse effects and tolerability. Primary Care Companion to the Journal of Clinical Psychiatry, 3(1), 22–27. https://doi.org/10.4088/pcc.v03n0105
Gabriel, F. C., de Melo, D. O., Fráguas, R., Leite-Santos, N. C., Mantovani da Silva, R. A., & Ribeiro, E. (2020). Pharmacological treatment of depression: A systematic review comparing clinical practice guideline recommendations. PloS One, 15(4), Article e0231700. https://doi.org/10.1371/journal.pone.0231700
Gautam, S., Jain, A., Gautam, M., Vahia, V., & Grover, S. (2017). Clinical Practice Guidelines for the management of Depression. Indian Journal of Psychiatry, 59(5), 34–50. https://doi.org/10.4103/0019-5545.196973
Jakobsen, J. C., Katakam, K. K., Schou, A., Hellmuth, S. G., Stallknecht, S. E., Leth-Møller, K., Iversen, M., Banke, M. B., Petersen, I. J., Klingenberg, S. L., Krogh, J., Ebert, S. E., Timm, A., Lindschou, J., & Gluud, C. (2017). Selective serotonin reuptake inhibitors versus placebo in patients with major depressive disorder. A systematic review with meta-analysis and Trial Sequential Analysis. BMC Psychiatry, 17(1), Article 58. https://doi.org/10.1186/s12888-016-1173-2
Moreno-Agostino, D., Wu, Y.-T., Daskalopoulou, C., Hasan, M. T., Huisman, M., & Prina, M. (2021). Global trends in the prevalence and incidence of depression:a systematic review and meta-analysis. Journal of Affective Disorders, 281, 235–243. https://doi.org/10.1016/j.jad.2020.12.035
Santarsieri, D., & Schwartz, T. L. (2015). Antidepressant efficacy and side-effect burden: A quick guide for clinicians. Drugs in Context, 4, Article 212290. https://doi.org/10.7573/dic.212290
Provided and edited by the members of MARI Research, Error in Medicine Foundation and MISMEDICINE Research Institute, including Gia D’Andrea, Rojina Nariman, and Dr. Pooya Beigi MD. MSc.