Misdiagnosis: Definition, Scope, Consequences, and Solutions in Healthcare
Misdiagnosis is a silent crisis in healthcare that affects millions of patients worldwide. It occurs when a health condition is incorrectly identified, leading to a wrong, missed, or delayed diagnosis. In simple terms, a misdiagnosis means the clinician got it wrong—either naming the wrong illness, overlooking the illness entirely, or discovering it much later than ideal.
This comprehensive article explores what misdiagnosis is, how and why it happens in both general medicine and mental health, the far-reaching consequences on individuals and society, and the latest research and initiatives aimed at preventing misdiagnosis. We also highlight real-world case studies and examine how organizations like the Misdiagnosis Association and Research Institution (MARI) are working to reduce diagnostic errors and improve patient outcomes.
Although modern medicine has achieved incredible feats, diagnostic errors remain alarmingly common. Multiple national reports estimate that most people will experience at least one meaningful diagnostic error in their lifetime. In the United States alone, studies suggest roughly 12 million outpatients each year receive a wrong or delayed diagnosis, and recent analyses estimate hundreds of thousands of serious harms—including permanent disability and death—are linked to misdiagnosis annually.
Why is misdiagnosis so pervasive? Diagnosis isn’t always straightforward: symptoms overlap, presentations vary, and time pressures or system constraints can force quick decisions. Cognitive biases (mental shortcuts), incomplete data gathering, and communication breakdowns can all lead a well-meaning clinician astray. Patients, too, may have atypical presentations or face language and cultural barriers. Misdiagnosis can occur in any field of medicine and in mental health, and it carries grave consequences—medically, psychologically, and socially.
Despite the scale of the problem, there is hope. Researchers, clinicians, and organizations like MARI are developing multifaceted strategies—spanning education, technology, teamwork, and patient engagement—to reduce diagnostic errors. The goal of this article is to provide a clear, informative overview that serves both healthcare professionals and the general public.
Misdiagnosis — What It Means and Why It Matters
Misdiagnosis in healthcare refers to any situation where a patient’s condition is not correctly identified in a timely manner. The umbrella term includes:
- Wrong diagnosis (incorrect diagnosis): a specific but wrong label is assigned (e.g., heart attack mistaken for indigestion).
- Missed diagnosis: the illness is present but not identified at all.
- Delayed diagnosis: the correct diagnosis is eventually made, but only after a harmful delay.
These categories often overlap. A missed diagnosis can later become a delayed diagnosis; an initial wrong label implies the real condition was missed. All constitute diagnostic error when there was an opportunity to make the correct or timely diagnosis but it didn’t happen.
Misdiagnosis can occur in any setting—primary care, emergency departments, specialty clinics, hospitals, and mental health care. Not every error causes harm, but many do, ranging from unnecessary treatments to life‑threatening delays.
Misdiagnosis — How Common Is It?
Estimating prevalence is challenging, but research shows misdiagnoses are distressingly common. U.S. outpatient studies suggest ~5% of adult visits involve a diagnostic error—roughly 12 million people annually. The National Academy of Medicine has noted that most people will experience at least one significant diagnostic error in their lives.
Globally, no healthcare system is immune. Factors that drive error—cognitive bias, system constraints, communication gaps—exist everywhere. Moreover, analyses focused on serious harm indicate that hundreds of thousands of patients each year suffer permanent disability or death from diagnostic errors, underscoring the scale of the problem.
Beyond human suffering, the economic costs are substantial: unnecessary tests and treatments, prolonged hospitalizations, malpractice litigation, and lost productivity create a large financial burden on health systems and society.
Misdiagnosis in Medicine — Common Types, Causes, and Examples
Across general medicine, certain patterns recur. Serious conditions frequently involved in misdiagnosis include cancers, vascular events (e.g., stroke, pulmonary embolism), and serious infections—sometimes referred to as the “Big Three.” These conditions can present with nonspecific symptoms and are easily mistaken for benign issues, yet delays can be catastrophic.
Dermatology offers illustrative pitfalls: skin cancers such as melanoma are sometimes dismissed as benign lesions; inflammatory dermatoses can be mistaken for infections. Cardiovascular misdiagnoses include heart attacks in women being attributed to anxiety or indigestion due to atypical presentations. Overlapping clinical pictures—like Lyme disease, chronic fatigue syndrome, and mononucleosis—also fuel diagnostic confusion.
Why do these happen? Common causes include cognitive biases (availability, anchoring, premature closure), incomplete history or examination, misinterpretation of tests, overconfidence, and narrow differentials. System factors—short visit times, limited access to tests or specialists, poor follow‑up of results—compound risk. Communication issues and language barriers further increase the chance of error.
Misdiagnosis in Mental Health — Challenges and Frequent Errors
Diagnosing mental health conditions relies on clinical interviews and subjective reports rather than definitive lab tests. Overlapping symptoms across disorders (e.g., mood change, anxiety, sleep disturbance) create fertile ground for error.
A classic pitfall is bipolar disorder misdiagnosed as major depressive disorder—especially when hypomanic symptoms are subtle or unreported. Anxiety disorders and physical illnesses can masquerade as one another; for example, panic attacks vs. cardiac arrhythmias or endocrine disease. ADHD and autism in adults are often missed or mislabeled, particularly in women and minorities.
Stigma, comorbidity, cultural and language differences, and variable clinician training add complexity. The consequences of psychiatric misdiagnosis can be profound: inappropriate medications, delayed effective therapy, and significant social and self‑identity impacts.
Misdiagnosis — Consequences for Patients and Society
Medical consequences: worsening of the true illness, harm from wrong treatments, preventable complications, and unnecessary procedures. Infectious misdiagnoses can fuel community spread.
Psychological and emotional consequences: distress, trauma, erosion of trust in clinicians and the system, and stigma—especially with incorrect psychiatric labels.
Societal and economic consequences: billions in wasteful spending, malpractice burden and defensive medicine, public health impacts, and lost productivity and opportunity.
Preventing Misdiagnosis — Research and Practical Strategies
Reducing misdiagnosis requires a multi‑front strategy addressing human and system factors.
Education & training: structured clinical reasoning, awareness of biases, diagnostic timeouts, and case‑based learning.
Cognitive aids & decision support: checklists, clinical decision support systems, and judicious use of AI/ML; repeat/confirmatory testing when needed.
Communication & teamwork: robust handoffs, closed‑loop follow‑up of results, multidisciplinary reviews, and easy access to second opinions.
Patient partnership: thorough history sharing, symptom timelines, asking “what else could this be?”, understanding expected illness course, and seeking second opinions when needed.
System improvements: better access to care and specialists (including telemedicine), smarter EHR alerts and tracking, error‑reporting and learning systems, and policies that prioritize diagnostic safety.
Cultural change—embracing diagnostic humility, transparency, and learning from error—is the connective tissue enabling these tactics to work in practice.
Misdiagnosis — Real-World Case Studies and Lessons
- Case 1: Missed appendicitis labeled as a “stomach virus,” leading to rupture and severe infection—lesson: avoid premature closure; re‑evaluate worsening pain.
- Case 2: Type 1 diabetes in a child misdiagnosed as Type 2; wrong therapy caused dangerous instability—lesson: confirm critical distinctions with appropriate tests.
- Case 3: Changing skin lesion assumed benign; later confirmed melanoma with metastasis—lesson: biopsy or refer uncertain lesions promptly.
- Case 4: Bipolar disorder mislabeled as unipolar depression; antidepressant monotherapy worsened mood cycling—lesson: always screen for past mania/hypomania.
- Case 5: Pulmonary embolism mistaken for a panic attack in a patient with anxiety history—lesson: don’t let psychiatric labels overshadow evaluation of red‑flag symptoms.
Misdiagnosis — How MARI Research Is Addressing the Problem
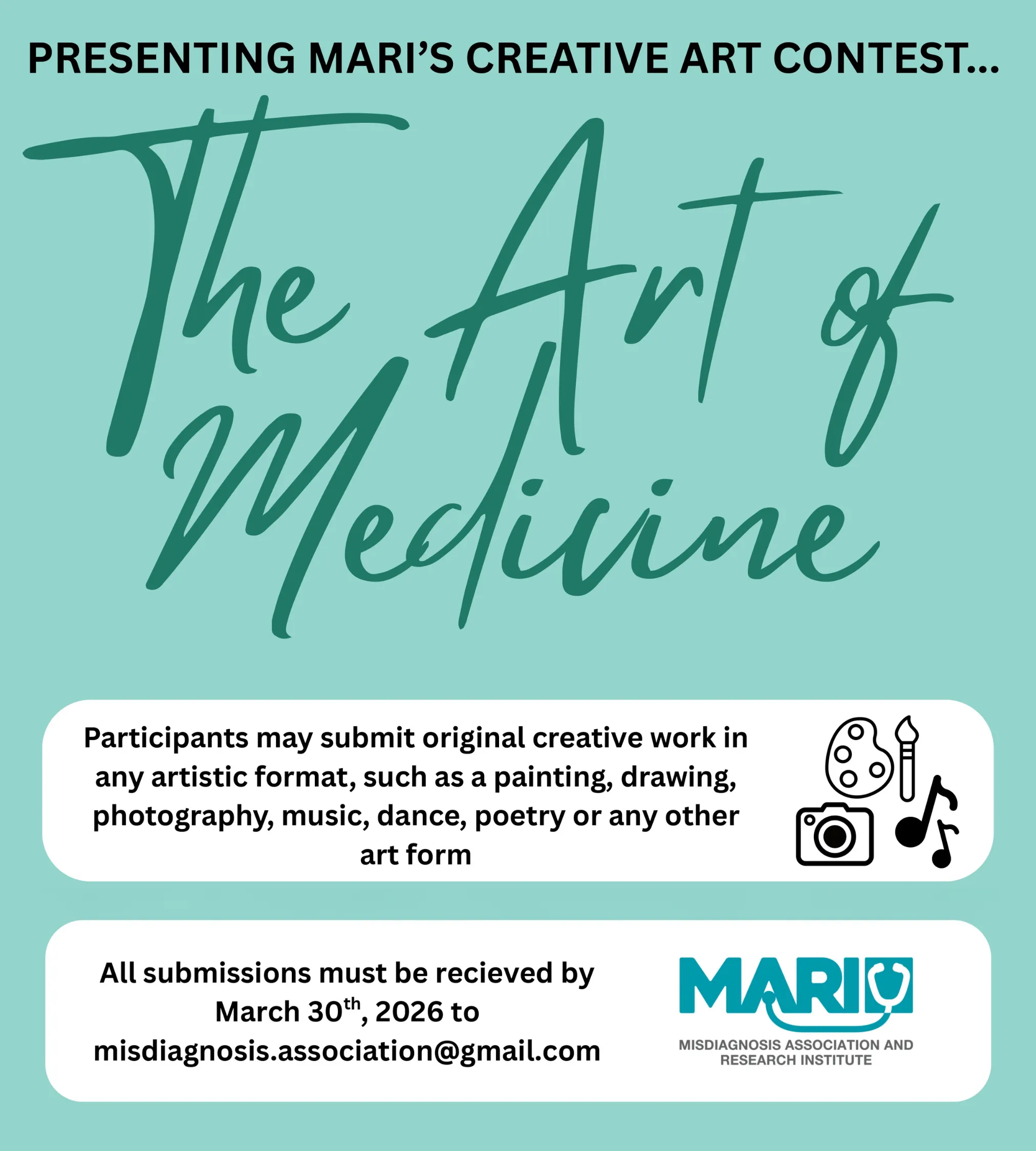
The Misdiagnosis Association and Research Institution (MARI) focuses on reducing diagnostic errors through research, education, and advocacy. Key contributions include:
Concise, high‑yield clinical summaries for providers, paired with plain‑language resources for patients.
Tools and checklists designed to counter diagnosis bias and broaden differentials.
Interdisciplinary initiatives across medicine, law, technology, nutrition, and veterinary care to share best practices.
Collaborations with academic and healthcare partners to study causes and solutions, and to promote a culture of transparency and learning.
By educating clinicians and empowering patients, MARI helps bridge information gaps and supports more accurate, timely diagnosis worldwide.
Misdiagnosis — Conclusion and Path Forward
Misdiagnosis is a widespread, high‑impact patient safety issue—but it is reducible. By combining stronger clinical reasoning, supportive technologies, robust systems and teamwork, and active patient partnership, healthcare can meaningfully lower both the frequency and severity of diagnostic errors.
Every patient deserves an accurate and timely diagnosis. With sustained effort from clinicians, patients, health systems, and organizations like MARI, the silent crisis of misdiagnosis can be transformed into a story of continuous learning and measurable improvement.
Sources (Selected)
Select references (representative): National Academy of Medicine (Improving Diagnosis in Health Care), studies on diagnostic error prevalence and harm; research on cognitive biases and system factors; primary care detection studies for mental health; and case reports illustrating consequences and prevention strategies.
1) What is Misdiagnosis, and how is it different from a missed or delayed diagnosis?
Answer: Misdiagnosis is an umbrella term that covers three situations: a wrong diagnosis (naming the incorrect condition), a missed diagnosis (failing to identify a present condition), and a delayed diagnosis (eventually correct, but too late to prevent harm). In practice they overlap: a missed diagnosis today often becomes a delayed diagnosis tomorrow; a wrong label implies the real condition was missed. Clinically, all three matter because they can lead to inappropriate treatment, disease progression, avoidable complications, and loss of trust. In quality programs, these scenarios fall under diagnostic error and should be measured, reviewed, and learned from.
2) Why does Misdiagnosis happen even with experienced clinicians and modern technology?
Answer: Diagnosis is probabilistic, not binary. Cognitive biases (anchoring on the first idea, availability from recent cases, premature closure), incomplete data (rushed history/exam), system constraints (short visits, fragmented records), and communication gaps (handoffs, lost results) all contribute. Technology helps but can also create alert fatigue or over-reliance on a single test. The best antidote is a combination of structured reasoning (broad differentials, “What else could this be?”), closed-loop follow-up of abnormal results, and teamwork—plus a culture where uncertainty can be acknowledged rather than covered.
3) Which conditions are most commonly linked to harmful Misdiagnosis?
Answer: The “Big Three” categories account for most serious harm: vascular events (e.g., stroke, pulmonary embolism), infections (e.g., sepsis, meningitis), and cancers (e.g., lung, colorectal, melanoma). They often present with nonspecific symptoms (dizziness, fever, fatigue, weight loss, chest pain) that mimic benign issues. High-impact specialties include emergency medicine, primary care, neurology, oncology, and dermatology. Because time-to-treatment is critical, errors here carry disproportionate risk of disability or death.
4) How can patients personally reduce the risk of Misdiagnosis?
Answer: Come prepared with a timeline of symptoms, key past history, meds/supplements, exposures (travel, ticks, pets), and family history. Describe the worst symptom first, what makes it better/worse, and “the moment you were last well.” Ask your clinician: “What else could this be?”, “What red flags should trigger me to return?”, and “When should I expect improvement?” Seek a second opinion if symptoms persist or treatment doesn’t match the clinical picture. Keep copies of results, and use patient portals to confirm abnormal findings were addressed.
5) What can clinicians do day-to-day to prevent Misdiagnosis without doubling their workload?
Answer: Adopt micro-habits: (1) Generate 3 plausible alternatives before closing the chart. (2) Run a brief checklist: does anything not fit? what’s the worst-case? what test/result would change my mind? (3) Document diagnostic uncertainty and a concrete follow-up plan. (4) Use decision support for unfamiliar presentations and high-stakes differentials. (5) Close the loop on tests/referrals with task lists or EHR reminders. These steps add minutes but save hours of rework and risk downstream.
6) Does Misdiagnosis happen more in mental health, and why?
Answer: Yes—psychiatric diagnosis relies on interviews and behavior, not definitive labs. Symptom overlap (depression vs bipolar; PTSD vs anxiety; ADHD vs anxiety/trauma; autism vs personality disorders) and stigma/under-reporting complicate accuracy. A classic pitfall is bipolar misdiagnosed as unipolar depression, especially when hypomanic periods are brief or perceived as “good days.” Screening for past mania/hypomania, systematic use of validated tools, collateral history, and re-assessment over time markedly improve accuracy.
7) How does Misdiagnosis affect patient trust and adherence?
Answer: A wrong or late label can feel like betrayal. Patients may disengage, skip follow-ups, or doctor-shop, which paradoxically raises risk of further error. Trust rebounds when clinicians are transparent about uncertainty, explain their reasoning, and invite questions. Apologizing for an error, correcting course, and outlining a safety-net plan (what to monitor, when to return) restore therapeutic alliance and reduce harm.
8) What role does bias play in Misdiagnosis (gender, race, language, mental-health labels)?
Answer: Diagnostic overshadowing (attributing new symptoms to an existing psych label), gender bias (atypical MI in women called anxiety), and language/culture barriers (somatic idioms) are well-documented contributors. Use trained interpreters, ask open, non-leading questions, and verify understanding via teach-back. Build structured pathways for high-risk complaints (chest pain, neuro deficits, fever with hypotension) that minimize subjective bias in disposition decisions.
9) Can AI and decision support eliminate Misdiagnosis?
Answer: AI/CDSS reduce variance and surface rare but relevant differentials, especially in imaging and dermatology, but they don’t replace clinical reasoning. Their value peaks when (a) integrated into workflow, (b) explainable, (c) used on the right questions (pattern recognition, risk stratification), and (d) paired with follow-up protocols. Over-trusting a model or ignoring discordant clinical data can create new failure modes. Think “co-pilot,” not “autopilot.”
10) How should a clinic measure Misdiagnosis without punitive vibes?
Answer: Track signals rather than blame: 72-hour returns to ED with diagnosis change, unexpected ICU transfers, pathology/radiology discordance, abnormal result without documented follow-up, cancer stage at diagnosis vs expected benchmarks. Review anonymized cases in regular diagnostic M&M sessions. Celebrate saves (near-misses caught by safety nets). Share actionable fixes (new order set, checklists, result-tracking tweaks), and re-measure.
11) Misdiagnosis vs. overdiagnosis: are they the same?
Answer: No. Misdiagnosis = wrong/missed/delayed identification of the actual condition. Overdiagnosis = correctly labeling a condition that would never cause harm in the patient’s lifetime (e.g., some indolent cancers), often leading to overtreatment. Both harm patients and waste resources, but the remedies differ: better calibration and shared decision-making for overdiagnosis; better reasoning, testing, and follow-up for misdiagnosis.
12) What are practical “red flags” patients should know to avoid catastrophic Misdiagnosis?
Answer: Seek urgent care for: sudden neurologic deficits (weakness, speech/vision changes), worst headache of life, chest pain with shortness of breath, fainting with exertion, fever with confusion or stiff neck, rapidly evolving rash, unintentional weight loss, new or changing skin lesion, and severe abdominal pain with guarding. If discharged, ask: “Which specific dangers were ruled out, and how?” and “What exact signs should bring me back immediately?”
13) How does Misdiagnosis appear in dermatology and what should primary care do?
Answer: High-risk pitfalls include melanoma mistaken for benign lesions, cellulitis vs inflammatory mimics (gout, eczema, stasis dermatitis), and drug eruptions vs viral exanthems. Primary care should use the ABCDE rule for pigmented lesions, low threshold for biopsy/referral for evolving lesions, and photo-documentation for interval change. For “cellulitis,” check distribution, bilateral edema, and systemic signs; when in doubt, derm consult/tele-derm avoids unnecessary antibiotics/admissions.
14) How does Misdiagnosis intersect with infections and sepsis?
Answer: Early infection often looks like a benign viral syndrome. Delays arise when vitals and risk factors aren’t integrated or abnormal labs aren’t tracked. Use sepsis screens (qSOFA/NEWS2), repeat vitals, and time-boxed re-assessment (e.g., in 2–4 hours). “Viral” shouldn’t be a discharge-and-forget label—give clear return precautions, especially for the elderly, immunocompromised, postpartum patients, and those with implanted devices.
15) What’s the right approach to chest pain to minimize Misdiagnosis?
Answer: Treat chest pain as a process, not a moment. Obtain ECG/troponins with proper serial testing, risk stratify (HEART score), and look for mimics (PE, aortic dissection, pericarditis, esophageal causes). Beware atypical presentations in women, diabetics, and older adults. Discharge requires explicit safety-netting: expected course, medication adherence, follow-up within 24–72 hours, and precise return triggers.
16) How should clinicians communicate uncertainty to prevent Misdiagnosis and preserve trust?
Answer: Say what you know, what you don’t, and what you’ll do next. Example: “Based on X and Y, pneumonia is most likely; here’s our plan. Two things still concern me—if A or B occurs, come back immediately. I’ve ordered Z to close the loop.” This frames uncertainty as professional vigilance, not incompetence, and aligns patient and clinician on a shared monitoring plan.
17) How can health systems build “safety nets” against Misdiagnosis at scale?
Answer: Implement result-tracking dashboards (no abnormal critical value without action), return-visit triggers for high-risk complaints, automated referral aging reports, and diagnostic timeouts in order sets (e.g., syncope, dizziness, fever, chest pain). Expand tele-specialty access (derm, neuro, ID, psych). Run diagnostic M&M monthly with cross-disciplinary participation and publish fix lists with owners and deadlines.
18) What should a patient do after a suspected Misdiagnosis?
Answer: Document your course (dates, symptoms, meds), request your records (notes, labs, imaging), and schedule a second opinion with a relevant specialist. Bring a concise one-page summary and ask the new clinician to start from first principles. If harm occurred, consider a medical ombudsman or patient advocate. The primary goal is clinical correction—legal routes are separate and time-sensitive but shouldn’t delay needed care.
19) Where does MARI Research fit in the global effort to reduce Misdiagnosis?
Answer: MARI focuses on practical education and research: high-yield clinician summaries, patient-facing explainers, bias-countering checklists, and multi-disciplinary collaborations (medicine, law, tech, nutrition, veterinary). By improving the quality of information exchange on both sides of the stethoscope and promoting culture change (humility, transparency, learning), MARI helps translate evidence into fewer errors, earlier right diagnoses, and better outcomes.