Malaria: A Comprehensive Guide to Symptoms, Diagnosis, Treatment, and Prevention
Objective: This article aims to educate healthcare professionals, patients, and at-risk populations on malaria’s diagnosis, treatment, and prevention strategies to improve disease management.
Clinical Diagnosis and Differential Diagnosis
Introduction
Malaria is caused by protozoan parasites from the genus Plasmodium, with Plasmodium falciparum and Plasmodium vivax being the most important species affecting humans. The disease is transmitted through the bite of infected Anopheles mosquitoes and is endemic in 84 countries, leading to approximately 250 million clinical cases and 620,000 deaths annually. Vulnerable populations include young children, pregnant women, and individuals with no prior immunity, such as refugees, travelers, and immigrants.
Mechanism of Infection
Malaria infection begins when an infected Anopheles mosquito bites a human, injecting Plasmodium sporozoites into the bloodstream. These sporozoites travel to the liver, invade hepatocytes, and mature into schizonts. Upon rupturing, schizonts release merozoites into the bloodstream, where they invade red blood cells (erythrocytes). Inside erythrocytes, the parasites undergo asexual replication, leading to cycles of cell rupture and further merozoite release. Some merozoites differentiate into gametocytes, which can be taken up by another mosquito during a blood meal, continuing the transmission cycle.
Symptoms of Malaria
Common Symptoms
- Fever
- Chills
- Sweats
- Headaches
- Dizziness
- Nausea
- Muscle aches
- Fatigue
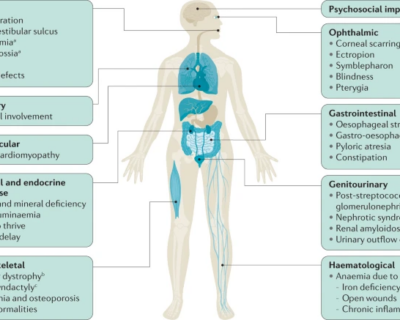
Severe Symptoms
- Cerebral Malaria: Seizures, confusion, and coma.
- Respiratory Distress: Difficulty breathing due to pulmonary edema or metabolic acidosis.
- Severe Anemia: Life-threatening reduction in red blood cells.
- Organ Failure: Kidney or liver failure, which can be fatal without immediate treatment.
Clinical Diagnosis and Differential Diagnosis
Diagnostic Methods
- Clinical Assessment: Evaluation of symptoms such as fever, chills, and fatigue. However, this method has low accuracy due to symptom overlap with other diseases.
- Microscopy/Blood Smear Test: The gold standard for malaria diagnosis, involving the examination of a blood sample under a microscope to detect Plasmodium parasites.
- Rapid Diagnostic Tests (RDTs): Detect specific malaria antigens or enzymes in the blood. Less sensitive than microscopy, especially in cases with low parasite density.
- Polymerase Chain Reaction (PCR) Testing: Highly sensitive method for detecting Plasmodium DNA. Accurate but costly and impractical in resource-limited settings.
Differential Diagnosis
Malaria must be differentiated from other causes of fever, such as bacterial enteric fever, meningitis, dengue, yellow fever, and viral hepatitis. In children, common differentials include respiratory infections, bacterial bloodstream infections, and gastroenteritis.
Treatment of Malaria
Antimalarial Medications
- Artemisinin-based Combination Therapies (ACTs): First-line treatment for malaria, combining artemisinin derivatives with other antimalarials to improve efficacy and reduce resistance.
- Chloroquine: Used for P. falciparum, P. knowlesi, and P. malariae infections, though resistance limits its use in some regions.
- Quinine and Quinidine: Used for severe malaria but limited by toxicity and resistance.
- Primaquine: Eliminates dormant liver stages of P. vivax and P. ovale to prevent relapse.
Severe Malaria Treatment
Intravenous or intramuscular artesunate is recommended for severe malaria due to its rapid action in clearing parasitemia. Supportive care, including fluid management, blood transfusions, and mechanical ventilation, may be necessary for complications such as anemia, respiratory distress, or organ failure.
Drug Resistance
Drug resistance, particularly in P. falciparum, is a growing concern. Resistance to chloroquine, ACTs, mefloquine, and primaquine has been reported, driven by factors such as inadequate dosing, incomplete treatment courses, and the genetic adaptability of the parasite.
Prevention of Malaria
Vector Control Measures
- Indoor Residual Spraying (IRS): Coating indoor surfaces with insecticides to kill mosquitoes. Requires trained personnel for effective application.
- Insecticide-Treated Nets (ITNs): Provide a physical barrier and kill or repel mosquitoes. More effective than untreated nets.
- Untreated Nets (UNs): Offer limited protection as a physical barrier but do not kill mosquitoes.
Personal Protection for Travelers
- Prophylactic Medications: Atovaquone-proguanil, doxycycline, or mefloquine.
- Clothing: Wear full-length, light-colored, and insecticide-treated clothing in malaria-endemic areas.
Vaccination
The RTS,S/AS01 (Mosquirix) vaccine, targeting the pre-erythrocytic stage of P. falciparum, has moderate effectiveness and is recommended for children in areas with moderate to high malaria transmission. Multiple vaccine candidates are under development, offering hope for better prevention strategies.
Resources and Support
Conclusion
Malaria remains a major global health issue, particularly in tropical and subtropical regions. Despite advancements in diagnosis, treatment, and prevention, the disease continues to cause substantial morbidity and mortality. Effective control strategies, including vector control, personal protection, prophylactic medications, and vaccination development, are essential. However, the emergence of drug-resistant Plasmodium strains and insecticide-resistant mosquitoes underscores the need for continued research and innovation.
References
Bria, Y. P., Yeh, C., & Bedingfield, S. (2021). Significant symptoms and nonsymptom-related factors for malaria diagnosis in endemic regions of Indonesia. International Journal of Infectious Diseases, 103, 194-200. https://doi.org/10.1016/j.ijid.2020.11.177
Buck, E., & Finnigan, N. A. (2023). Malaria. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551711/
Croft, A. M. (2010). Malaria: prevention in travellers. BMJ Clinical Evidence, 2010, 0903. https://pmc.ncbi.nlm.nih.gov/articles/PMC3217660/
Fikadu, M., & Ashenafi, E. (2023). Malaria: An overview. Infection and Drug Resistance, 16, 3339-3347. https://doi.org/10.2147/IDR.S405668
Hanson, J., et al. (2014). The fluid management of adults with severe malaria. Critical Care, 18(6), 642. https://doi.org/10.1186/s13054-014-0642-6
Hyde, J. E. (2007). Drug-resistant malaria – an insight. The FEBS Journal, 274(18), 4688-4698. https://doi.org/10.1111/j.1742-4658.2007.05999.x
Ippolito, M. M., et al. (2021). Antimalarial drug resistance and implications for the WHO global technical strategy. Current Epidemiology Reports, 8(2), 46-62. https://doi.org/10.1007/s40471-021-00266-5
Pinheiro, L. C. S., et al. (2018). Current antimalarial therapies and advances in the development of semi-synthetic artemisinin derivatives. Anais Da Academia Brasileira De Ciências, 90(1 Suppl 2), 1251-1271. https://doi.org/10.1590/0001-3765201820170830
Poespoprodjo, J. R., et al. (2023). Malaria. The Lancet, 402(10419). https://doi.org/10.1016/s0140-6736(23)01249-7
Stanisic, D. I., & Good, M. F. (2023). Malaria vaccines: Progress to date. BioDrugs, 37(6), 737-756. https://doi.org/10.1007/s40259-023-00623-4
Tizifa, T. A., et al. (2018). Prevention efforts for malaria. Current Tropical Medicine Reports, 5(1), 41-50. https://doi.org/10.1007/s40475-018-0133-y
Venugopal, K., et al. (2020). Plasmodium asexual growth and sexual development in the haematopoietic niche of the host. Nature Reviews Microbiology, 18(3), 177-189. https://doi.org/10.1038/s41579-019-0306-2
Wangdi, K., et al. (2018). Comparative effectiveness of malaria prevention measures: A systematic review and network meta-analysis. Parasites & Vectors, 11(1), 210. https://doi.org/10.1186/s13071-018-2783-y
White, N. J. (2022). Severe malaria. Malaria Journal, 21(1), 284. https://doi.org/10.1186/s12936-022-04301-8
Provided and edited by the members of MARI Research, Error in Medicine Foundation and MISMEDICINE Research Institute, including Rojina Nariman, Helia Falahatkar and Dr. Pooya Beigi MD. MSc.