Errors in Treatment: Understanding Medication Related Errors and Its Impacts
Common Causes of Treatment Errors
Introduction
Errors in treatment, specifically those involving medication related errors, continue to be a significant risk within the healthcare system. Currently, medication errors are one of the most common and preventable sources of patient injury (Tariq et al., 2022). The main issue is that these errors can occur at multiple stages in patient care, including prescription, dispensing, and administration, making them increasingly difficult to prevent. Common issues include incorrect dosage, drug, route, pharmacy-related errors, and wrong-patient incidents. Additionally, patients not adhering to medication instructions can contribute to errors (Tariq et al., 2022).
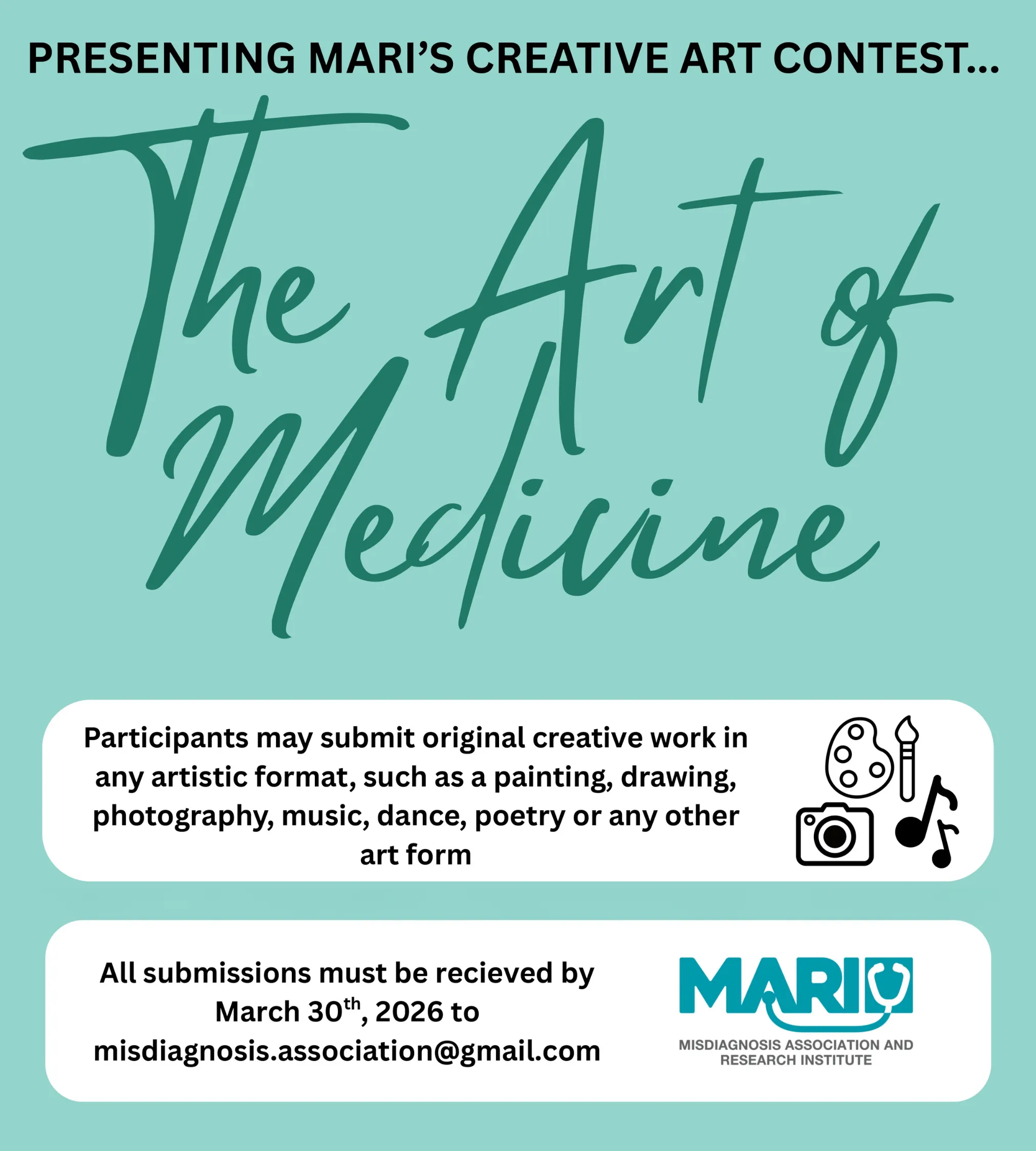
According to Dr. Pouya Beigi, founder of MARI (Misdiagnosis Association and Research Institute), medication errors are a major contributor to medical mistakes and can lead to adverse health outcomes, such as poor treatment results (Beigi, 2024). This article will explore the common causes, consequences, and preventive measures for medication-related errors, emphasizing the importance of accurate diagnosis, effective therapeutic communication with patients and their healthcare teams, proper patient education, and adherence to medication guidelines.
Common Causes of Treatment Errors
Medical errors are increasingly becoming a public health concern, as they are now the third leading cause of death among hospitalized patients in the United States (Rodziewicz et al., 2023). Because medication errors are seen as preventable due to multiple safeguards in place at the hospital, it is important to educate on medication errors once patients are back home as there are less safeguards in place (Tariq et al., 2022). Medication errors account for 22% of hospital readmissions after discharge (Tariq et al., 2022).
Patient Non-Adherence to Medication Instructions
One of the most common causes of treatment errors is patient non-adherence to prescribed medication regimens. Patients may forget to take their medication, misinterpret instructions, struggle with resource limitations, or intentionally skip doses due to side effects or a perceived improvement in their condition (Jimmy & Jose, 2011).
Adherence to long-term therapy in developed countries averages only 50% among chronic disease patients, while half of these individuals intentionally do not take their medications as prescribed. The other 50% are either unaware that they are not following the regimen correctly or find the regimen too complicated (Jimmy & Jose, 2011). All these factors contribute to ineffective treatment, decreased quality of life, and disease progression.
Healthcare Provider Miscommunication and Verification of Understanding
Miscommunication between healthcare providers and patients can result , inappropriate treatments, and inadequate patient education (Rodziewicz et al., 2023). Dr. Beigi (2024), emphasizes the importance of clear communication, beginning with patients providing all relevant information that could be important to their healthcare providers to ensure a proper diagnosis and subsequential treatment regimen is being made.
Another factor is the patient’s ability to read and comprehend medication instructions. If patients misunderstand these instructions, they may take their medication incorrectly, thus having a treatment error (Jimmy & Jose, 2011). Studies show that healthcare providers are not properly verifying if patients are understanding their medication regimen (Jimmy & Jose, 2011). Between 40% and 60% of patients cannot recall sufficient details about how and when to take their medication just 10–80 minutes after being educated. Additionally, 60% of patients show almost immediate misunderstanding of their instructions following an educational session with their healthcare provider (Jimmy & Jose, 2011).
Pharmacy-Related Medication Errors
Pharmacy errors can be categorized as either judgmental or mechanical. Judgmental errors occur due to a failure to recognize potential drug interactions, inadequate patient counseling, incomplete drug usage review, or inappropriate patient screening (Tariq et al., 2022). Mechanical errors occur during dispensing and preparation, such as incorrect instructions or providing the wrong dose, strength, or quantity (Tariq et al., 2022). Leading to As a result, the patient will take taking medications that should either not be taken or an alternative should have been given.
Impacts of Treatment Errors
The consequences of medication errors can range from minor side effects to severe complications, including death. These impacts affect not only patients but also healthcare providers.
Adverse Health Outcomes
Medication errors can result in adverse drug reactions, decline of the patient’s condition, or even death (Makary & Daniel, 2016). Misdiagnosis, as highlighted by Dr. Beigi and MARI, can lead to inappropriate treatment, potentially causing further harm rather than recovery (Beigi, 2024).
Emotional and Psychological Impact
Patients who experience treatment errors may suffer from emotional distress, trauma, anxiety, and loss of trust in the healthcare system (Rodziewicz et al., 2023).
Healthcare providers involved in medication errors may also experience psychological distress, including guilt, anger, and even suicidal ideation, compounded by the fear of legal implications (Rodziewicz & Hipskind, 2023).
Preventive Strategies
Preventing treatment errors require approaches involving patients, healthcare providers, and pharmacies.
Enhancing Patient Education
Educating patients about their medications, including proper usage, potential side effects to be aware of, and the importance of adherence, is a key strategy to reduce treatment errors (Rodziewicz et al., 2023). According to Jimmy & Jose (2011), through the following preventative strategies, medication error can decrease:
- Simplifying medication regimens and actively involving patients in decision-making.
- Providing patients with written instructions detailing how, when, why, and for how long they should take their medications.
- Offering adherence tools such as calendars or medication containers with notifying when the last dose was taken.
- Assessing adherence during follow-up appointments, identifying barriers, and addressing them to improve compliance. Ensuring to update the patient on these changes will improve adherence to their medication.
Improving Communication Amongst Healthcare Providers and Encouraging Error Reporting
Creating a cohesive communication strategy among healthcare providers is essential for accurate diagnosis and appropriate treatment planning. Standardized handoff protocols, comprehensive patient records, and drug usage reviews can enhance information sharing and reduce treatment errors (Aljabari & Kadhim, 2021).
Additionally, creating a supportive environment where healthcare providers feel safe to report errors is important. Due to the potential repercussions associated with errors in healthcare, many studies indicate that underreporting is a significant issue (Aljabari & Kadhim, 2021).
References
Aljabari, S., & Kadhim, Z. (2021). Common Barriers to Reporting Medical Errors. The Scientific World Journal, 2021, 6494889. https://doi.org/10.1155/2021/6494889
Beigi, P. (2024). Why Your Skin Issue Might Be Misdiagnosed! Dr. Beigi’s Insights Retrieved from https://www.youtube.com/watch?si=SFf65obTCSqLpTg-&v=yA7PpiNM600&feature=youtu.be
Tariq RA, Vashisht R, Sinha A, et al. Medication Dispensing Errors and Prevention. [Updated 2024 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519065/
Jimmy, B., & Jose, J. (2011). Patient medication adherence: measures in daily practice. Oman medical journal, 26(3), 155–159. https://doi.org/10.5001/omj.2011.38
Makary, M. A., & Daniel, M. (2016). Medical error—the third leading cause of death in the US. BMJ, 353, i2139.
Rodziewicz, T. L., Houseman, B. T., & Hipskind, J. E. (2023). Medical error prevention. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK499956/
Provided and edited by the members of MARI Research, Error in Medicine Foundation and MISMEDICINE Research Institute, including Bukky Alausa, Helia Falahatkar and Dr. Pooya Beigi MD. MSc.