Diagnostic Errors in Women’s Sexual and Reproductive Health
Introduction
A woman with a demanding schedule that includes full-time work, caregiving responsibilities, and regular community involvement has been quietly managing chronic reproductive health symptoms for years. When she seeks care from her primary care provider, her ability to remain outwardly functional leads to reassurance rather than investigation. Her concerns are not perceived as urgent. Further diagnostic evaluation is deferred. Believing the symptoms are normal, she carries on, accommodating her life around the discomfort. Over time, these discomforts begin to interfere with daily life. When her condition is eventually identified, it has progressed to a stage requiring more complex intervention.
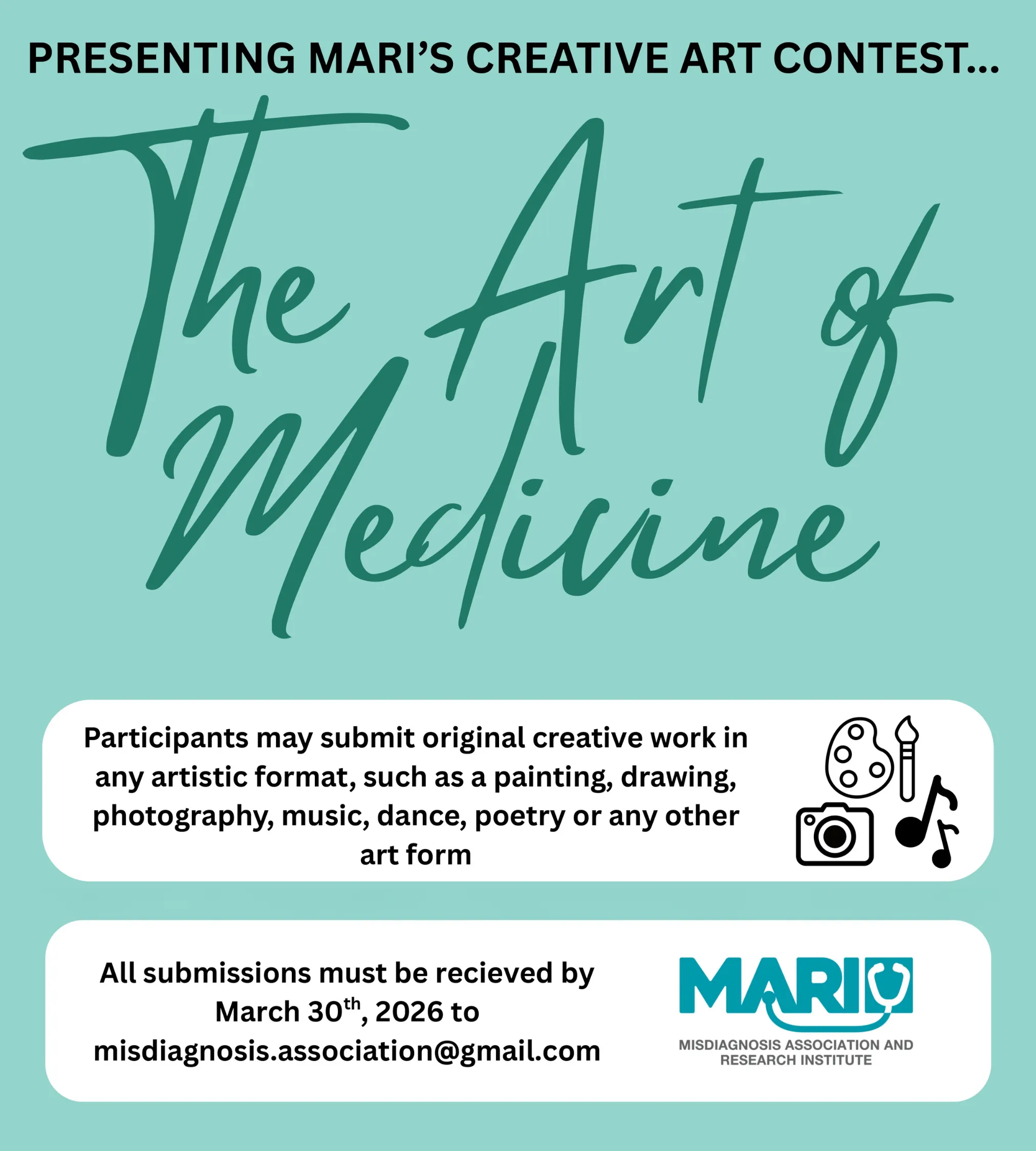
This article examines diagnostic errors in women’s sexual and reproductive health in primary care and how these failures reflect mismedicine, a term coined by Dr. Pooya Beigi, founder of the Misdiagnosis Association and Research Institute (MARI), to describe medical actions and system-level gaps that cause harm or fail to meet the standard of care (Blissy, 2024). For many women, diagnostic error does not appear as a single identifiable error. It unfolds as a prolonged period of uncertainty, normalization of symptoms, and delayed recognition of harm. By centering women’s experiences, this article highlights how diagnostic errors emerge and how these patterns shape patient safety in everyday healthcare.
What Diagnostic Error Looks Like for Women
Diagnostic uncertainty is one of the main contributors to diagnostic error across medicine (Alam et al., 2017). Diagnostic error refers to a diagnosis that is delayed without good reason, incorrect, or missed entirely (Singh et al., 2019). In women’s sexual and reproductive health, diagnostic error most often takes the form of delay. Not one misstep, but many small ones.
Uncertainty is especially common in primary care, where symptoms may be vague, develop gradually, or overlap with common conditions, making diagnosis more difficult (Alam et al., 2017). For women, this uncertainty is often experienced as repeated reassurance. Advice is given to wait and see, even as concerns persist or evolve. When symptoms are addressed one visit at a time, women may move through the healthcare system without a clear sense of whether their experiences warrant further investigation. Unresolved issues remain unresolved.
Why Diagnostic Delay Matters
Timely and accurate diagnosis is central to good medical care and is the first step toward achieving the best possible health outcomes (Singh et al., 2019). For women, delayed diagnosis often means years of unmanaged pain, disruption to daily life, and lingering uncertainty about whether their experiences are legitimate or concerning.
In primary care, diagnostic delays are often influenced by system-level factors such as delayed testing, poor communication, and inadequate follow-up of persistent symptoms (Singh et al., 2017). These gaps accumulate across visits. Symptoms are treated as isolated complaints rather than recognized as part of a broader pattern. As articulated by Dr. Pooya Beigi, mismedicine emphasizes how diagnostic problems can sometimes stem from a series of justified decisions (Blissy, 2024). For women, harm often develops quietly and is shaped by repetition.
Women’s Sexual and Reproductive Health: Patterns of Missed Recognition
In women’s sexual and reproductive health, common symptoms include painful menstrual periods, painful sexual intercourse, and chronic pelvic pain. These symptoms may present as pain in the lower abdomen, hips, lower back, and thighs. They are often accompanied by nausea, vomiting, diarrhea, fatigue, headaches, and dizziness (Nagy & Khan, 2023). Although these symptoms can be severe, they are frequently treated as routine. This makes it harder for women to distinguish between what is expected and what warrants further care.
Gender bias further shapes how symptoms are interpreted. Women’s pain and reproductive health concerns are more likely to be normalized or attributed to stress, hormonal changes, or lifestyle factors (Samulowitz et al., 2018). This can minimize their perceived significance and allow serious conditions to be reframed as routine experiences. In healthcare systems, unconscious gender biases can influence how patients are treated, especially when women continue to function despite ongoing symptoms. Because general practitioners are often the first point of contact and play a key role in determining when specialist care is pursued, early interpretations can carry lasting consequences. As a result, women’s concerns may be perceived as less urgent, reinforcing the assumption that what they are experiencing is normal.
This can place the burden on women to self-manage symptoms rather than prompting timely investigation.
Reducing Harm and Supporting Safer Diagnosis
Delays in diagnosis can be reduced through education, updated guidelines, and the use of diagnostic tools in primary care (De Kok et al., 2024). Effective information sharing between general practitioners and specialists supports continuity of care and safer outcomes for women experiencing ongoing pain (Nagy & Khan, 2023). Clear follow-up matters. Coordinated care matters. Attention to evolving symptoms matters.
Additionally, involving patients more actively in their care can also reduce diagnostic delays. When women understand which symptoms to monitor, know when to follow up, review test results, ask questions, and have access to their medical records, they are better positioned to support timely diagnosis and reduce the risk of harm (Singh et al., 2017).
Conclusion
Diagnostic errors in women’s sexual and reproductive health often develop gradually within primary care. They take shape through uncertainty, normalization of symptoms, and fragmented care. Women who continue functioning while managing persistent pain or discomfort may be especially vulnerable to delayed recognition of serious conditions. Viewed through the framework of mismedicine, these patterns reflect system-level failures rather than isolated mistakes (Blissy, 2024). Addressing these failures requires continued action informed by evidence. Further research is needed to better understand how often diagnostic errors occur, what factors contribute to them, and which interventions are most effective. Strengthening continuity, communication, and follow-up offers a practical path forward. Together, these efforts can help interrupt patterns of delay and improve patient safety for women over time.
References
Alam, R., Cheraghi-Sohi, S., Panagioti, M., Esmail, A., Campbell, S., & Panagopoulou, E. (2017). Managing diagnostic uncertainty in primary care: a systematic critical review.
BMC Family Practice, 18(1). https://doi.org/10.1186/s12875-017-0650-0 Blissy. (2024, August 9). Why Your Skin Issue Might Be Misdiagnosed! Dr. Beigi’s Insights | The Blissy Experience Ep. 10. YouTube.
De Kok, L., Henk Schers, Boersen, Z., Braat, D., Teunissen, D., & Nap, A. (2024). Towards reducing diagnostic delay in endometriosis in primary care: a qualitative study. BJGP Open, 8(3), BJGPO.2024.0019–BJGPO.2024.0019. https://doi.org/10.3399/bjgpo.2024.0019
Nagy, H., & Khan, M. A. (2023). Dysmenorrhea. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560834/
Samulowitz, A., Gremyr, I., Eriksson, E., & Hensing, G. (2018). “Brave Men” and “Emotional Women”: A Theory-Guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Research and Management, 2018(1), 1–14. https://doi.org/10.1155/2018/6358624
Singh, H., Graber, M. L., & Hofer, T. P. (2019). Measures to improve diagnostic safety in clinical practice. Journal of Patient Safety, 15(4), 311–316. https://doi.org/10.1097/pts.0000000000000338
Singh, H., Schiff, G. D., Graber, M. L., Onakpoya, I., & Thompson, M. J. (2017). The global burden of diagnostic errors in primary care. BMJ Quality & Safety, 26(6), 484– 494. https://doi.org/10.1136/bmjqs-2016-005401
Provided and edited by the members of MARI Research, Error in Medicine Foundation and MISMEDICINE Research Institute, including Erika Schaller, Rojina Nariman, and Dr. Pooya Beigi MD. MSc.