OVARIAN CANCER
Dr.Lovepreet Singh
INTRODUCTION
In most of the world’s regions, cancer is the leading cause of death and currently the biggest impediment to obtaining an acceptable life expectancy. The third most frequent gynecologic cancer after uterine and cervical cancer and ovarian cancer. Additionally, it has the highest fatality rate and the poorest prognosis.
Ovarian cancer is three times more deadly than breast cancer while having a lower prevalence. Most instances are discovered when the disease has already progressed, resulting in dismal consequences. The limited predictive value of the current screening tests adds to this anguish. Despite the most advanced ongoing clinical trials and the introduction of new treatment modalities in recent years, ovarian cancer continues to be one of the most deadly malignancies in women. The lack of successful methods for the early detection of ovarian cancer is largely to blame for the poor clinical outcome.
Additionally, there is evidence of care that deviates from recommended guidelines, possibly as a result of clinical variation seen in the treatment of ovarian cancer.

Epidemiology
The incidence of ovarian carcinoma is greater in high-income countries compared to middle and low-income countries.
Etiology
- Ovarian cancer is associated with a number of risk factors. It primarily affects postmenopausal women, and as women get older, their incidence, stage, and reported survival rates of the disease all rise.
- Age – Epithelial ovarian cancer is primarily thought to affect postmenopausal women and is an age-related condition. Women over 65 years old have a more noticeable increase in the incidence of this cancer.
- Menstrual-related factors- Based on many studies, ovulation without interruption can contribute to the incidence of ovarian cancer by damaging the epithelium of ovaries.
- Parity- According to the findings of numerous studies, pregnancy may have a protective effect against ovarian cancer. Women who have a live birth or an induced abortion have a lower risk of developing ovarian cancer, and this risk declines as more live births occur.
- Age at childbirth- Results of a may studies indicates that older age in pregnancy is associated with a decreased risk of ovarian cancer

- Pelvic inflammatory disease- An increase in the release of cancer cells in the tissues surrounding the ovary is linked to ovary inflammation-related events (such as repairing the damaged ovary).
- Endometriosis- Ovarian cancer risk is increased by endometriosis. Compared to other types of ovarian cancer, endometriosis-associated ovarian cancer is found earlier and in less advanced stages.
- Family history-A family history of breast or ovarian cancer is the most significant risk factor for ovarian cancer. An increased risk of ovarian cancer is linked to a personal history of breast cancer. Women who have a history of breast, uterine, or ovarian cancer in their mother or sister are more likely to develop the disease themselves.
- Lifestyle factors/Nutrition and diet- A higher intake of cholesterol is linked to an increased risk of ovarian cancer, which can be decreased by eating more vegetables, vitamin supplements, beta-carotene, and B-complex vitamins. A plant-based diet is crucial for lowering the risk of cancers linked to hormones because it protects against the development of ovarian cancer.
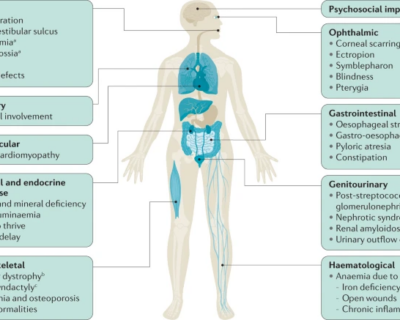
History and Physical Symptoms
Ovarian cancer symptoms are non-specific, making it simple to overlook them at an early stage because they can be attributed to other potential disease processes. Frequently, the symptoms don’t show up until they reach the late stage (stage III or stage IV). Abdominal fullness, bloating, nausea, abdominal distention, early satiety, fatigue, changes in bowel habits, urinary symptoms, back pain, dyspareunia, and weight loss are among the symptoms that can be pr esent in the patient of ovarian cancer. The symptoms are vague months before ovarian cancer is discovered.

Screening and diagnosis
Due to the lack of specific symptoms in patients, it is very challenging to make an early diagnosis of ovarian cancer, which lowers patient survival rates. Medical history and physical examination are the first steps in evaluating ovarian cancer along with complete blood count checks for anemia and Bbood chemistry tests to check kidney and liver function
According to the International Federation of Gynecologists and Obstetricians (FIGO) committee imaging is a crucial factor in determining the extent and location of ovarian cancer spread and determining the best course of treatment. Imaging tools that are frequently used include ultrasound, computed tomography (CT) scans, and magnetic resonance imaging (MRI). Additionally, a physical examination and transvaginal ultrasonography are used to diagnose tumours, and exploratory laparotomy is used to determine the origin of ovarian cysts. Combining a serum HE4 test or CA125 test with the Symptoms can improve the screening for ovarian cancer.
The imaging is typically done in conjunction with the measurement of CA-125 levels. Only 50% of early-stage epithelial ovarian cancers have elevated CA-125, but this is true of the majority of epithelial ovarian cancers overall. Other physiological or benign pathological conditions like endometriosis, pregnancy, ovarian cysts, and inflammatory peritoneal diseases are also associated with elevated CA-125 levels. As a result, research on additional biomarkers is currently being done to increase the specificity of ovarian cancer biomarkers.
Treatment
Surgery alone often has the ability to treat the disease without adjuvant chemotherapy in low-risk cases that are detected in the early stages. However, patients with high-grade disease staging are found to benefit from a combination of chemotherapy. At this time, it is discovered that the effect of adjuvant therapy is determined more by the tumour’s grade and stage rather than its type. However, chemotherapy may have some unfavourable side effects, including nausea, vomiting, menopause, mouth sores, hand and foot rashes, and infertility.
Prognosis
The prognosis of ovarian cancer is directly dependent on the disease stage at the time of diagnosis. The 5-year survival rate falls to 80% in women with disease that has spread to nearby tissues and 25% in those with metastatic disease.